Maternal Fetal Medicine Unit Delivers Joy to Ghanaian Mothers
Mariam* is soft spoken as she recalls the three miscarriages that led her to seek care at the newly established Maternal Fetal Medicine (MFM) unit at Tamale Teaching Hospital (TTH) in Ghana.
“I came here when I was 30 weeks due to…bad obstetric history and low birthweight. When I came here they were monitoring me, encouraging me and giving me hope.”
As she looks to the corner where TTH midwife Ikmatu Titiaka is holding a sleeping baby, she smiles, straightens and says proudly, “I have my baby here. He’s fine. He’s healthy.”
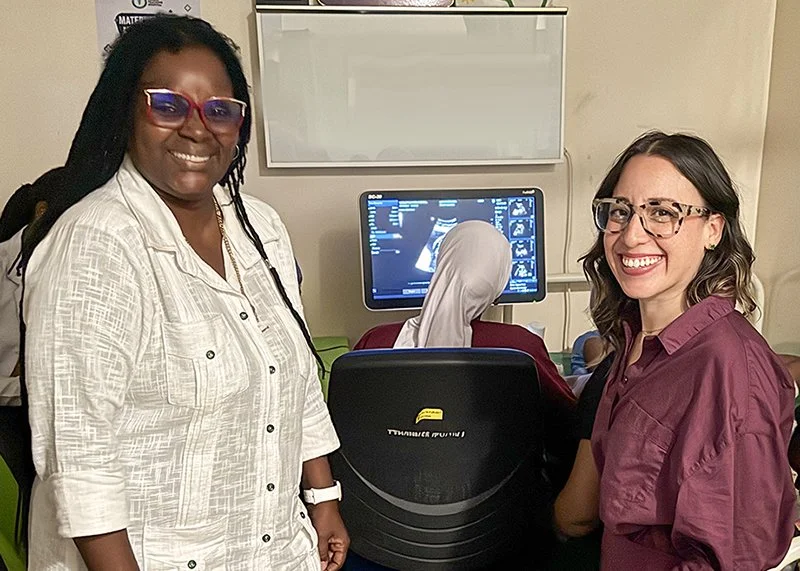
Dr. Ana Maria Simono Charadan and Dr. Sasha Hernandez worked together to develop the Maternal Fetal Medicine Unit at Tamale Teaching Hospital through the AMPATH Ghana partnership.
Little Abdul-Aziz* does not yet realize the joy and relief that his arrival has brought to his family. “Our women in the Northern Region here, we value giving birth so much,” explained Ikmatu. “We cherish having kids a lot. If you are married or you have your partner, and then you don't have babies, it can even lead to divorce.”
“The care I had here has helped me a lot. Financially, emotionally, socially and physically,” Mariam said. “They're always at their work, encouraging us to come for the scan and the dopplers. So I'm grateful to them and they should continue their good work. May God bless them all. All of them. They are good.”
The tiny unit sees 15-16 cases per day with just two beds.
The MFM unit at TTH provides high-quality, evidence-based, contextualized support to women with high-risk pregnancies due to conditions such as hypertension, diabetes, sickle cell anemia or fetal anomalies.
The unit works out of a very small room in TTH. With just two beds, they see between 15-16 cases per day for ultrasounds (scans), dopplers (a special ultrasound to check the health of the placenta), non-stress tests and cardiotocography (CTG) to monitor fetal heart rate and contractions.
TTH is the sole tertiary referral hospital in a region serving Northern Ghana with a population of more than 7 million people. Many of the expectant mothers are referred from facilities across the vast catchment areas the hospital serves which are mostly rural. The incidence of high-risk pregnancies in TTH’s catchment area is very high including high rates of pregnancy-related hypertension.
"The new Maternal-Fetal Medicine Unit at Tamale Teaching Hospital is a great opportunity for our mothers and babies-as well as our residents,” said Dr. Amoako Asirifi, head of the Department of Obstetrics and Gynecology at TTH and the University for Development Studies (UDS) in Ghana. “It will help us provide better care and also train our young doctors to handle complicated cases with confidence. This is a big step forward for the health of our community."
The MFM unit, which opened in August 2023, is one of the first initiatives from the AMPATH Ghana partnership between TTH and UDS in Ghana, and New York University Grossman School of Medicine (NYUGSOM) leading the partnership on behalf of the AMPATH Consortium. Dr. Ana Maria Simono Charadan was head of the Obstetrics and Gynecology Department at TTH when Dr. Sasha Hernandez, an obstetrician and gynecologist from NYUGSOM, arrived in Tamale in 2022 as the first reproductive health team leader for AMPATH Ghana.
“I was writing a proposal (for an MFM unit) for many, many years on my computer,” Dr. Ana Maria said. “But this proposal was archived or filed in my computer (waiting for the right opportunity). I told Dr. Sasha about this…and she said we’re able to do that because we (AMPATH) had done a program like that in Kenya.”
“One of the key priorities for the AMPATH Ghana partnership, specifically in women's reproductive health, was improving ultrasound access and management for both our pregnant and non-pregnant women,” said Dr. Sasha. The two doctors initially started with training doctors and midwives on the use of ultrasound, but the resulting evidence-based recommendations led to the development of the MFM unit. The MFM unit started with two midwives and now has four to address the increase in patient demand.
“The unit, I think, is just such a beautiful success story to partnership, to the power of partnership,” added Dr. Sasha. “We did not get any grant funding to start this. This was literally like, ‘Let's just make it happen. Let's see what happens.’ We've been lucky to have some small research funding now go into the unit. But this is proof that you don't always need money to start things. It's just that passion and that drive of people coming together to improve maternal health care, global health equity, and just really the lives of the women here in Northern Ghana.”
“We are giving better services, quality of services to our patients,” Dr. Ana Maria said. “They need it. Our population, female population, need quality of services, need the doctor to be sitting in the consultation to see them, to make the correct diagnosis, to discuss the correct management to treat well. This is what they need. And we are ready to do that. It's true, we are living in this country with low income, but it doesn't mean that we cannot make it. We can make it.”
Dr. Ah-Lam Abdul-Kadir Napari is one of more than 10 specialists in the Obstetrics and Gynecology Department that work on five rotating teams to provide care in the MFM unit during the week and on an emergency basis on weekends. “It's been excellent in the sense that most of the scans we usually get from peripheral facilities don't really give us the details we need in order to manage the patient thoroughly. But having an MFM unit in our department has helped us tailor our diagnosis. So it's been very beneficial to us.”
“Maternal Fetal Medicine has changed the life of so many people. I could count and count,” said Donyuo Sukyiriyele Sylvia, one of the inaugural midwives of the unit. “Because of our guidelines for the unit, we are able to intervene immediately or intervene properly. I think it has helped a lot of people to have their babies instead of getting intrauterine fetal deaths and other morbidities.” She explained that many high-risk mothers need to be monitored weekly or even bi-weekly and the unit offers reduced or waived fees for repeat tests to encourage mothers to maintain the necessary schedule.
“The feedback, you can carry.”
The MFM team has begun research to quantify the impact of the unit on maternal and newborn outcomes at TTH, but Millicent Amma Kumassey, the deputy director of nursing for the Obstetrics and Gynecology Department at TTH, says the impact is obvious. “The feedback, you can carry,” she said, referring to babies in their mothers’ arms. “They are glorious. Now they have their live babies and they themselves, they are very fine. So they come in appreciating and even tell others about it.”
“The best part of my job is just seeing that the mothers come out safely, that they deliver safely and they have their babies in their arms,” said Ikmatu. “That's so fulfilling and touching for me because the goal is to make sure that we reduce the number of stillbirths and we are achieving that.”
Nurse Charles Timumpi has continued to volunteer with the MFM unit after completing a mandatory year of national service while he awaits his permanent posting. “I'll go to town and I'll meet a woman and she'd say, ‘I know you. I have met you at the MFM. You've done a scan for me.’ It's just the joy that I get in helping somebody to be happy. That's just what motivated me and I’m still with MFM.” He hopes to land a permanent position in the MFM unit when his nursing class receives their postings through the national system.
Unfortunately, with high-risk pregnancies, not all outcomes are positive. “Recently one of the moms that lost her baby came back to thank us and just say, thank you for the care you delivered and thank you for trying your best and being on top of what you do, even though I didn't get to take my baby home,” recalled Dr. Sasha. “So I think we've had so many success stories where we have saved a lot of babies and improved the care of moms. We have. But that is still a reminder that we're not going to save every baby. They're high-risk pregnancies for a reason. We're still going to have some bad outcomes. But it's that impact that you're making woman to woman, person to person, and that they come back and thank you, is so good.”
Education continues to be a main focus of the unit and trainees rotate through the unit as space allows. Each new batch of students, house officers (new doctors) and residents participate in training. “Every day, every day, every day,” said Dr. Ana Maria.
The Maternal Fetal Medicine Unit at Tamale Teaching Hospital which serves a population of more than 7 million people.
Dr. Odinaka Emmanuella Anara is a resident in obstetrics and gynecology in her second year of the three-year program. She received ultrasound training from Dr. Hernandez and is now on the rotating schedule to provide scans at the unit. “It was exciting. Something we didn't know how to do before, and then all of a sudden in a short duration, we were able to use the probe to scan and then see if there are any abnormalities.”
One of the unit’s goals is to bring this service and evidence-based care to other health facilities in northern Ghana. The team recently trained two midwives from a neighboring hospital so they could share these skills and the MFM unit’s evidence-based algorithms with colleagues at their local facility.
Fifth-year medical student Juliana Opare-Duodu explained that as part of their rotations, each UDS medical student is supposed to rotate in the unit at least once per week, but the number is limited by the small size of the unit. “If they could accommodate more than one or two students in a day, we’d be very glad.”
Dr. John Bosco, a house officer, visits the unit whenever his schedule and space allow. “I mean, as part of human existence, we need one another. The love that they share inside the room is marvelous. That's what keeps me going and also the fact that anytime I go there, I have something new to learn.” He hopes to pursue a residency in obstetrics and gynecology and eventually return to his home village to provide care. “In the rural areas, you are your own boss, and if you've not received the basic knowledge during your house officer days, it will become an issue in the end.”
Everyone involved with the MFM unit dreams of an even brighter future with a bigger space and more resources. “Because as success started, the number keep increasing monthly, daily, weekly,” said Deputy Director of Nursing Kumassey.
With increased space also comes the opportunity to create a fellowship in maternal fetal medicine. Currently only a general obstetrics and gynecology fellowship is available in the region. Dr. Napari said there are at least two specialists interested in a future MFM fellowship. “I'm sure if the center is set up and then we get that accreditation, you have more than two join it. I might even consider also joining.”
“In summary, I can tell you that the Maternal Fetal Medicine unit is a great achievement. I know that maternal fetal medicine is making a lot of positive changes for the outcome of maternal and antenatal morbidity and mortality. We also know that maternal fetal medicine is increasing the skills for our specialists, our clinicians, midwives and nurses,” said Dr. Ana Maria. “Through AMPATH, my dream came true.”
With care from the TTH maternal fetal medicine unit, so did Mariam’s.
*Names have been changed for patient privacy